Despite its rapidly growing economy, China remains a low- and middle-income nation. An example of this is its healthcare system. Although China has made impressive strides in improving healthcare access for its population, the country still lags developed nations in tackling cervical cancer.
More cases of cervical cancer are diagnosed in China each year than in any other nation. China accounts for about 20 per cent of all cervical cancers diagnosed worldwide[1]. Even with more than 557 million women at risk of developing cervical cancer[2] and 402 million who are of screening age[3], China has no national cervical cancer screening program.
Rising cervical cancer rates and the lack of a nationwide cervical cancer screening program make cervical cancer a critical public health issue.
Cultural traditions impact screening
Chinese culture includes very old, deep-rooted traditions. China has been heavily influenced by Confucianism, which views sexual activity as having a primarily procreative purpose reserved for marriage[4].
These views shape the attitudes of many Chinese women today, particularly in rural regions, and have impacted the take-up of cervical cancer screening.
Most cervical cancers are caused by human papillomavirus (HPV)[5], which is a sexually acquired infection. Some women in China maintain expectations of ‘correct’ female behaviour and attach a social stigma to HPV because it is sexually transmitted. Therefore, some women are embarrassed to undergo cervical cancer screening. Consequently, cervical cancer screening is underutilised by Chinese women despite evidence that it can help detect early cancer5.
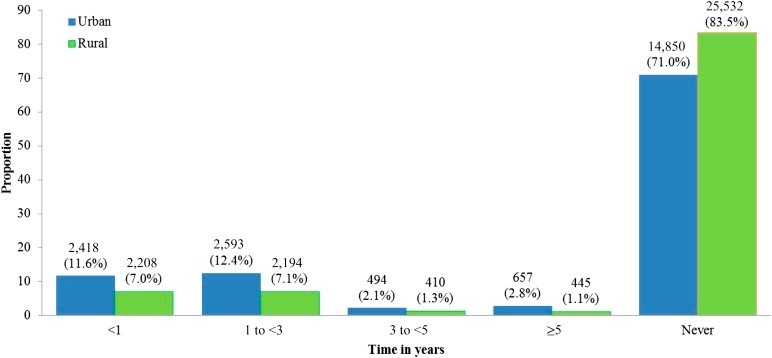
Prevalence and time since last Pap test by urban/rural status
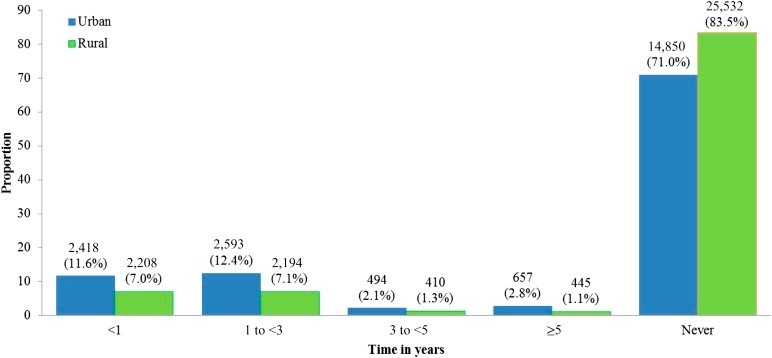
(Wang, B et all. 2015. ‘Cervical cancer screening among adult women in China 2010, The Oncologist. doi: 10.1634/theoncologist.2014-0303)
Ongoing cervical cancer crisis in young women
China’s economic boom and rapid urbanisation have resulted in significant lifestyle changes – mostly western influences – for women across the nation, especially young women.
These lifestyle changes have contributed to a rise in HPV infection rates and to higher cervical cancer rates among younger women throughout the country[6].
The lifestyle changes including younger ages for first sexual intercourse, more sexual partners and a take-up in smoking. The increase of women experiencing first full-term pregnancy at a younger age is also a factor in HPV progression[7].
China’s ageing population presents challenges
China’s rapidly ageing population presents unique challenges when it comes to fighting cervical cancer. Middle-aged women, who outnumber younger women in China3, can’t get immunisation against HPV due to the lack of programs available for their age group. Therefore, given the absence of HPV immunisation programs, cervical cancer screening is critical for preventing cervical cancer amongst them.
Studies suggest that if nothing is done to improve access to cervical cancer screening in China, the number of cervical cancer cases will continue to increase2.
Improved screening programmes are desperately needed to reduce the burden of cervical cancer and help secure the future of generations of Chinese women.
TruScreen recognises the important need for improved screening capabilities in China. TruScreen has NMPA (formerly CFDA) approval for use in China and, in partnership with an established distribution network, is currently working with the Chinese Obstetrics and Gynaecology Association (COGA) to roll out TruScreen’s innovative, real-time technology to those in need.
TruScreen has already commenced a large-scale evaluation with COGA to screen over 20,000 women in 100 top-tier public hospitals across 10 provinces in China. The COGA program has progressed positively, with 52 hospitals commencing screening so far. The evaluation results are expected in the 2021 financial year. TruScreen looks forward to sharing those results.
[1] Weim, et al, 2018, ‘Rising Mortality Rate of Cervical Cancer in Younger Women in Urban China’, J Gen Intem Med, vol. 34, no. 2, p.281-284, viewed 16 December, https://link.springer.com/content/pdf/10.1007%2Fs11606-018-4732-z.pdf
[2] HPV Information Centre, 2019, ‘China human papillomavirus and related cancers fact sheet, 2018’, ICO/IARC Information Centre on HPV and Cancer, https://hpvcentre.net/statistics/reports/CHN_FS.pdf
[3] Central Intelligence Agency, 2019, ‘The World Factbook’, https://www.cia.gov/the-world-factbook/
[4] Woo, J. Brotto, L. Gorzalka, B. 2009, ‘The Role of Sexuality in Cervical Cancer Screening Among Chinese Women’, Health Psychology, vol. 28, no.5, p.598-604, https://med-fom-brotto.sites.olt.ubc.ca/files/2014/12/Woo_Brotto_and_Gorzalka_2009.pdf
[5] Arbyn, M. Castellsague, X. de Sanjose, S. Bruni, L. Saraiya, M. Bray, F & Ferlay, J. 2011. Annals of Oncology, Volume 22, Issue 12, December 2011, pages 2675–2686, https://doi.org/10.1093/annonc/mdr015
[6] Weim, et al, 2018, ‘Rising Mortality Rate of Cervical Cancer in Younger Women in Urban China’, J Gen Intem Med, vol. 34, no. 2, p.281-284, viewed 16 December, https://link.springer.com/content/pdf/10.1007%2Fs11606-018-4732-z.pdf [7] Shi, J. Canfell, K. Lew, J. Qiao, Y. 2012, ‘The Burden of Cervical Cancer in China: Synthesis of the evidence’, International Journal of Cancer, vol. 130, p.641-652, viewed 16 December 2019, https://onlinelibrary.wiley.com/doi/pdf/10.1002/ijc.26042