How TruScreen’s real-time cervical cancer screening works

TruScreen’s breakthrough cervical cancer screening device is a viable and attractive alternative to traditional cervical screening methods. The TruScreen device resolves many of the ongoing issues associated with Pap tests, including failed samples, poor patient follow-up, patient discomfort, and the need for supporting laboratory infrastructure. It also resolves the problem associated with HPV testing, which tests for the much more prevalent HPV virus, and not the presence of pre-invasive cervical cancer states. These issues are particularly pertinent in low- and middle-income countries (LMICs) – key markets for TruScreen.
The development of the device was led by leading medical academics from Sydney University, Professor Malcolm Coppleson and Dr Bevan Reid, who sought to establish objective technology that improved upon the conventional Pap test. The researchers subsequently settled upon opto-electrical technology to detect cancerous cells on the cervix.
The TruScreen device is currently the only opto-electrical real-time cervical screening system certified for use in multiple LMICs.
How does the TruScreen device work?
The TruScreen device consists of a disposable Single Use Sensor (SUS), a Handheld Device (HHD), and an Intelligent Cradle (IC) which works together to detect and identify cancerous and precancerous changes to the cervix.
Firstly, a pen-like wand covered by a Single Use Sensor (SUS) is used to gently touch multiple spots on the cervix. The SUS contains a precision lens and electrodes which interfaces with the cervix. In doing so, it sends and picks up low level electrical and optical signals (14 readings per second) from the cervical tissue.
The TruScreen Handheld Device then acts as a microcomputer to analyse these signals and compares them to an integrated database of 2,000 patients drawn from a wide range of geographic and ethnic backgrounds with differing histological diagnoses. This analysis identifies the presence of abnormal (cancerous and pre-cancerous) cells in the cervix and provides physicians with real-time results.
Each TruScreen examination takes one to two minutes to produce results, compared to conventional Pap tests which can take days, weeks, or even months in some countries, for a result to be returned.
How does screening with the TruScreen device compare to other current practices?
The TruScreen device has been tested extensively in numerous studies around the world. Clinical studies have shown its performance is equal to, or better than, high-quality cytology tests.
The TruScreen device has been found to be twice as sensitive as the Pap test and significantly more sensitive than HPV DNA testing at defining high-grade cervical lesions in a real-world LMIC setting. Instant reporting also eliminates delays associated with transporting samples to laboratories for analysis, thus avoiding the risk of losing patient contact.
Unlike cytology-based screening which require laboratory infrastructure and involve high resource costs, the TruScreen device can be used effectively by medical or paramedical staff, with minimal training.
An ongoing study with the Chinese Obstetrics and Gynaecology Association (COGA) comparing TruScreen to Liquid-Based Cytology (LBC) and HPV DNA testing (HPV) showed TruScreen has exceeded expectations.
Interim results demonstrate TruScreen has a sensitivity of 89.29% (compared to 67.87% for Liquid-Based Cytology (LBC) and 92.86% for HPV tests) and a specificity of 87.17% (LBC 90.07%, HPV 87.17%). Sensitivity and specificity are measures of a test’s ability to correctly diagnose a disease. A high sensitivity results in fewer false negatives, and a high specificity results in fewer false positives in the screening process.
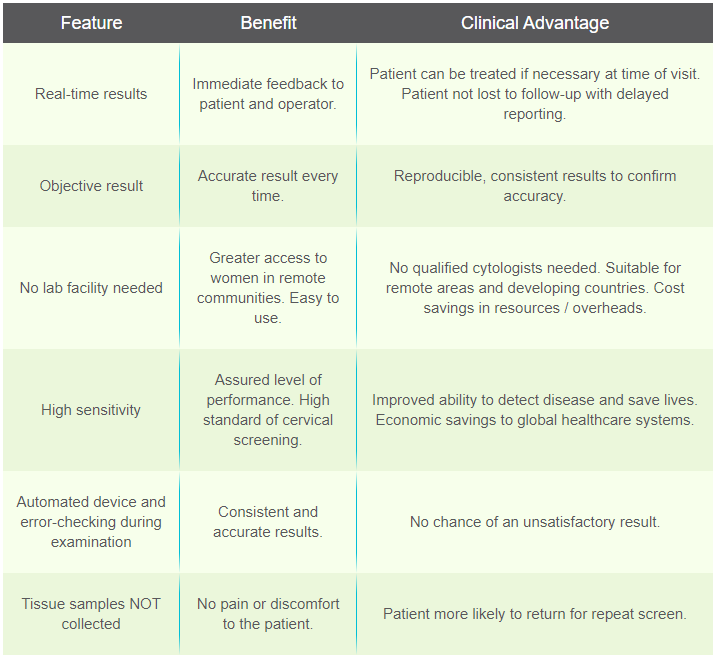
Features and benefits of the TruScreen device
The TruScreen device is not only an accurate system for cervical cancer screening, but importantly for LIMICs, it is a portable device that can be used with minimal training and without the infrastructure associated with traditional cytology screening tests.
Additionally, unlike Pap tests, the device does not collect tissue samples meaning patients experience minimal discomfort and pain. This means patients are more likely to return for repeat screenings thereby improving overall screening rates.
The table below outlines the key features, benefits and clinical advantages of the device.